More and more organizations are seeing the value of integrating a trauma-informed approach into their organizational culture!
At the 2022 National Association of Community Health Clinic (NACHC) Conference in Chicago, Andi Fetzner, PsyD, and Lori Chelius MBA/MPH presented a poster highlighting Eisner Health’s Journey Through Implementing Trauma Informed Care. It went so well that in 2023, NACHC invited Andi and and the Eisner Team, Deborah Lerner, MD, Dr. Chris Hillson, MD and Gretchen Gates, LCSW from NACHC to host a breakout in San Diego to share best practices and tips to help other community health centers start their own program. We reached 135 people total both virtually and in-person.
Worshop Description:
How Healthy Is Your Health Center? How to Promote a Trauma Informed Care Environment for Patients and Staff
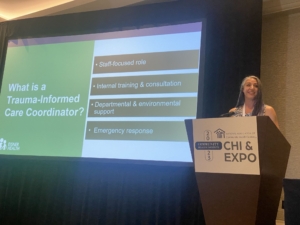
This workshop session will provide participants with the opportunity to learn how to create and sustain trauma informed environments for both health center patients and staff. Participants will hear from the Eisner Health team about their trauma informed care implementation journey. Participants will also learn about leadership and frontline staff roles in the implementation process and have hands on experience with tools that can be used every day in a variety of settings.
Some of the audience question/answers included:
How are trauma informed care coordinators funded?
Andi Fetzner – Eisner Health: At Eisner Health, the trauma-informed care coordinator position is a full-time position funded through a HRSA grant. In the first year, they utilized additional funding from a smaller grant to support an external organization to train and coach the internal position on the process of integrating a trauma-informed approach into the organization. State-based or foundation grants can support this approach to include current staff or similar, more part-time positions. Yet another approach other clinics have taken is to have a clinical provider in this role and split their time between patient encounters (billing supports the position) and TIC work (grant-funded).
What is the return on investment? What metrics are you tracking to measure effectiveness of this training?
Andi Fetzner – Eisner Health: The metrics thus far have not been tracked by our QI team but we notice a marked difference in the culture of the organization when people start to use the language of the training in meetings and other interactions. The initial motivation for bringing trauma-informed care into the organization was to decrease escalations. The feedback from staff and managers within the clinics is that the training has given them the language and skills to decrease the impact of stress and increase the ability to connect.
When you train your team members on trauma informed care, do you combine with motivational interviewing techniques or do you keep it separate?
Andi Fetzner – Eisner Health & Gretchen Gates – Enso Integrated Health: The recommendation is to keep these topics separate, especially when first starting to implement trauma-informed care and/or training. When we’re talking about trauma-informed care within a health center or system, we’re talking about culture shift, so it can take some time to build the foundational knowledge and internalize the practices. Even on the clinical side, the goal is to have everyone trained and speaking the language of TIC, as it’s more of a philosophy and way of providing care, while motivational interviewing is more of a discrete technique for clinical interventions.
Since self reflection and self awareness is so central to showing up for others, how can you help improve those skills for yourself and colleagues?
Gretchen Gates – Enso Integrated Health: The best first step can sometimes be just making the time to do it — whether it’s journaling, seeking therapy/counseling, or reading a book on trauma and thinking about its application to my life, I simply have to make the time and prioritize. I think we all are a little afraid to look in the mirror at our pasts, our experiences with trauma, or our biases so it’s easy to avoid. A simple way to start the reflection process is by taking one of the assessments we discussed during the session — either the Professional Quality of Life Scale or Buffalo Self Care Assessment. Either will give you a good idea of what’s going on and where to start to make some changes.
Andi Fetzner – Eisner Health: Past life experiences show up every day in present behavior. Acknowledging this fact helps create a culture where self-reflection and self-awareness are celebrated. While intervening in these moments and debriefing after them is helpful, I find the phrase an ounce of prevention can be worth a pound of cure relevant here. Do things that your future-self will thank you for doing. To me that means saying yes to some things and no to others. Eat breakfast. Ask for help (we have a hard time with this one as helpers). Do something that brings you joy just for fun like wearing a fun nail polish color or your favorite socks. Listen to a song you like. Sing in the car. Go for a walk. Lastly, I am an outdoorsy person and was happy to learn that even having a picture of a mountain or beach or landscape (if you can’t make it out during the day) can help balance one’s mood.
How do you de-stigmatize coping behavior, such as anger, while not enabling actual bad behavior?
Gretchen Gates – Enso Integrated Health: First, I operate under the principle (and share this with others) that everyone is doing the best they can with the knowledge, skills, and information they have at the time. This allows us to see patients and colleagues from a strengths-based and person-first perspective. Second, I view ANY coping, especially coping in the face or history of trauma, as a survival skill. Substance use and abuse, self-harm, running away, anger, pushing others away, overdependence, etc. can all be a learned way to survive an unhealthy situation. When we frame unhealthy coping in this way and provide psychoeducation on trauma and the fight/flight response, I find that people are much more likely to be compassionate with themselves, open to understanding the negative effects of this skill/response, and subsequently be more willing to consider alternative options.
Andi Fetzner – Eisner Health: We get asked this kind of question frequently related to holding people accountable for their actions. I mentioned in the presentation that there is no other approach that allows for people to be as accountable as a trauma-informed approach. As Gretchen mentioned, when a person has the space to understand their emotions, thoughts, and behavior, they can decide whether how they are acting is helpful or not in the current situation. The emotion of anger specifically can be explored and we can understand if there is a frustration, sadness, fear or something else happening. Once a person knows that they are safe to talk about their experience, they can access their whole brain and decide, learn, and think through their actions and reconnect with the team.
Read more about Eisner Health’s journey here:









 Getting Started: A Guide from Trauma to Resilience
Getting Started: A Guide from Trauma to Resilience